Review Article
Nano-formulations for Ophthalmic Treatments

Mahima John1 and Rajesh N Gacche2*
1D.Y. Patil Biotechnology and Bioinformatics Institute, Pune -411033 (MS), India2Department of Biotechnology, Savitribai Phule Pune University, Pune-411007 (MS), India
*Address for Correspondence: Rajesh N Gacche, Department of Biotechnology, Savitribai Phule Pune University, Pune-411007 (MS), India, Tel: +91-9423656179; Email: [email protected]
Dates: Submitted: 15 December 2017; Approved: 28 December 2017; Published: 29 December 2017
How to cite this article: John M, Rajesh GN. Nano-formulations for Ophthalmic Treatments. Arch Pharm Pharma Sci. 2017; 1: 028-035. DOI: 10.29328/journal.apps.1001005
Copyright License: © 2017 John M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Ocular Disorders; Drug Delivery; Polymers; Nanotechnology; Nano- formulations; Nano-carriers
Abstract
Ocular disorders encompass a multitude of diseases that are unique in their cause, therapy and degree of severity. Due to distinctive morphology of the eye, efficient ocular drug delivery has proven to be a difficult task. Current treatments of ophthalmological diseases include the usage of both intrusive as well as nonintrusive methods such as injections, eye drops, ointments, gels etc. The current state of the art drug delivery methods are associated with low bioavailability and therefore nanotechnology based drug delivery approached are evolving as for improving the therapeutic index of currently used drugs against variety of ocular disorders. This review highlights the recent developments in nano-formulations for ophthalmic treatment and also offers discussions towards the future prospectus of nano-formulations in the mainstream of ophthalmic diseases.
Introduction
Ophthalmology is a branch of medicine that focuses on handling the identification, treatment as well as prevention of diseases of the eye as well as the anatomy and the physiology of the overall visual system. Several diseases of the eye fall into the bracket of ophthalmology, and due to the delicate balance of the intricate structures that surround the eye, the visual system, as well as the eye itself, there can be a broad range of causes for these diseases. Some of them being: age, side effects of other diseases (such as diabetes), abnormalities in the brain that cause visual disturbances, as well as vision deficiencies that are present from birth such as color-blindness. Many diseases of the eye show no early symptoms, and often times it is only when vision has been impaired that patients notice a problem. By this stage the disease may have become quite advanced.
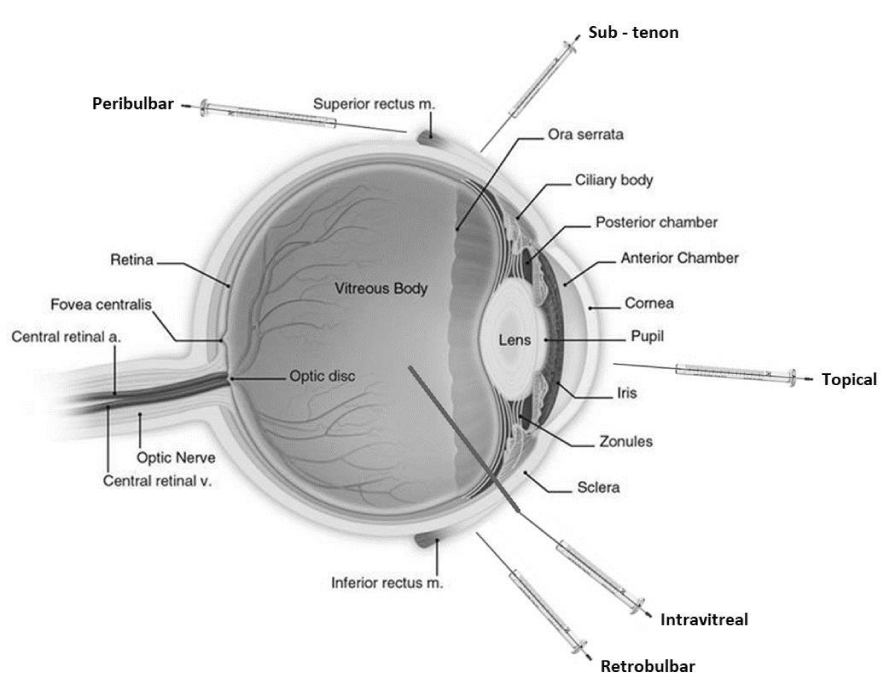
Therapeutic treatments such as eye drops, ointments, injections and implants have been the most extensively used remedy for the ophthalmic diseases but it is often disadvantaged by factors such as physiological barriers, enzymatic drug degradation, and nonspecific protein binding. The various routes of ocular drug administration are outlined in figure 1.
Nanoformulations are now being considered as potential alternatives for these traditional therapeutic treatments. Recent research studies demonstrated that nano-formulations can significantly enhance the therapeutic efficacy and bioavailability of ocular drugs, compared to the established classical ophthalmic drug delivery strategies [1]. There are over seventy different conditions relating to the eye that have been characterized as an ophthalmological disease. Some of the most recognized ophthalmic diseases that need to be prioritized for treating with nano approaches are described below.
Glaucoma
Glaucoma is an eye disease which causes damage to the eye’s optic nerve; it tends to gets worse over time. This condition is instigated by the build-up of pressure, called intraocular pressure, inside the eye. This pressure increase leads to damage in the optic nerve which is the nerve that sends image to the brain, therefore giving rise to impaired vision, and if not treated, can lead to permanent vision loss. This disease usually affects those who are above the age of 41 and does not favor any gender. Recently, there has been a large improvement of long term delivery systems such as hydrogel, nano-particles, nanoimplants and nanosized vesicle. This significant progress in nano-medicine has helped in the increasing improvement of anti-glaucoma medications [2].
Color blindness
Color blindness is usually hereditary and is less severe in its consequences in terms of loss of vision, therefore rather than a disease, it is referred to as a genetic condition. Some people also develop this condition as a side effect of an existing disease such as other eye diseases, multiple sclerosis, diabetes etc. This condition is brought about by a gene that is carried on the x chromosome and therefore affects more men than women. Women, who are often carriers of the trait, are most times not color blind themselves. Due to the incredible sensitivity of the eye, it is difficult to determine the specific cause of colour-blindness and as a result, the treatment of this disease is yet to be found. Nanotechnology based new methods for visualizing and targeting specific intracellular mechanisms within the eye are being developed and scientists are optimistic that color blindness in humans is a disease that can be cured with persistent research [3].
Diabetic retinopathy
Diabetes: a metabolic disease in which the blood sugar levels are high due to either inadequate insulin production or the body is unable to properly take action against the insulin. Diabetic patients are more prone for developing diabetic retinopathy. This disease is triggered because high blood sugar levels damage the blood vessels in the retina, ultimately causing cloudy vision. This disease usually affects those who have had diabetes for a long period of time and are over the age of 41.
The use of nanotechnology based strategies such as dendrimers and nano-particles have aided in drug delivery and as a result it is able to specifically target the affected area, in the case of diabetic retinopathy, this area would be the posterior segment of the eye. These new technologies have helped in decreasing the limitations of therapeutic drugs that are already being used to treat diabetic retinopathy [4].
Retinitis
Retinitis is a disease that affects the vision by damaging the light sensing tissue at the back of the eye called the retina. There is no known cure for this disease and therefore it is important that it is prevented as soon as patient shows signs of the symptoms of retinitis. This disease usually affects those from the ages 14 to 60+ at an equal likelihood. Nano-formulations such as nano-carriers are now being used to try to treat retinitis more efficiently as well as increase the bioavailability of the drug being used in order to increase the likelihood of the drug working [5].
Cataract
Cataract is a disease which leads to the clouding of the lens of the eye. This condensation of the eye leads to a blurriness, difficulty seeing at night, fading colours and in general, average decrease in vision. It has a gradual effect on the patient and can be avoided by protecting the eyes from the sun and refraining from smoking. The chances of developing a cataract largely increase after the age of 40 and are usually treated by surgery. Non-steroid anti-inflammatory drugs, natural antioxidants, biologic and chemical chaperones, and chaperones such as molecules have found great application in preventing and treating cataracts. Current scientific research on new treatment strategies such as nanotechnology will likely result in new anticataract agents. Nanotechnology together with biomimetic strategies will enable the development of next-generation, more efficient, less complex, and personalized treatments [6,7].
Myopia
Myopia, also known as near- sightedness, is an extremely common condition that affects a large amount of the population today. It is known to be caused due to extensive near vision tasks such as computer use. It is a condition that is corrected by the use of glasses, contact lenses or refractive surgery. Depending on the degree of myopia, the duration of time that the patient needs to use glasses or contact lenses differs. Myopia can affect people from ages ranging from even as young as 3 to 60+.
Macular degeneration
Macular degeneration is currently regarded as one of the leading causes of loss of vision. It is caused by the damaging of the retina. The macula is the centre of the retina and is responsible for focusing the central vision in the eye. This affects the ability to view things in fine detail, to recognize faces, read and perform other tasks that require concentration. This disease usually affects those around the ages of 30 to 60+. Obviously when it comes to macular degeneration, nanotechnology will be able to play a big role in its treatment, the promising new nano-formulations and will be better drug carriers and therefore can help in the increasing degradation of the retina. In the future, if macular degeneration is detected in the patient soon enough, it will be possible to stop the retina from reaching a stage in which a large amount of treatment is needed, essentially preventing the onset of macular degeneration [8]. The severity of ophthalmological diseases can only be determined by studying the specific disease that is in question. It can be determined form observing the above information that the severity of the diseases can vary from relatively harmless to extremely severe. It is essential that any possible uneasiness or symptom relating to the eye must be diagnosed immediately [9].
Challenges
The eye is a highly protective organ and its multiple physiological barriers make topical ophthalmic drug delivery a challenging area for formulation scientists [10]. One of the most widely employed current therapeutic treatments of ophthalmological disease is eye drops. Eye drops, although being non-invasive, have shown to have poor drug retention time. It is reported that ≤5% of drug in solution form is absorbed when administered topically [11], therefore the augmentation of this retention time has been widely explored. The lack of bioavailability in the ocular therapeutic treatments is and has been a cause of large concern in the field of ophthalmology. The primary cause of this absence has been found to be due to efflux transporters. Efflux transporters were found to be primary barriers leading to poor drug absorption and bioavailability, primarily for anterior segment ocular drug delivery [11].
Nano-formulations in ocular drug therapy
Nano-formulations have been brought into the field of ophthalmology in order to increase the bioavailability and therapeutic index of the drugs and thereby hopes of bettering the chances of patient’s recovery. Various forms of nano-formulations that has potential to be explored for treatment of ophthalmic disorders are described below.
Nano-particles
Nano-particles have been synthesised as targeted drug delivery systems. Nano-particles have proven to have low toxicity as well as long term stability. It is able to be mass produced and therefore it shows promise in terms of therapy. Nano-particles are mainly advantageous as compared to the ocular therapeutic counterpart due to its capacity for large bioavailability of drugs. When compared to the previous amount of bioavailability that was available with traditional ocular therapy, the nano-particle alternative is extremely favourable. Another advantage that nano-particles have is the ability to pass though barriers that conventional drugs cannot. For examples, calcium phosphate (CaP) nano-particles have shown great applications in drug delivery systems due to biocompatibility (non-toxic degradation products constitute the inorganic part of human hard tissue). As inorganic CaP nano-particles were found to be chemically stable, they were found to ensure the maintenance of desired pharmacological action [11].
Nano-emulsion
Emulsions are fine dispersions of infinitesimal droplets of two immiscible liquids. By definition, nano emulsions have dispersed phase in which the particle size is in the submicron or nanometer range. Nano-emulsions generally comprise of one or more amphiphilic lipid(s) or surfactants [1].To increase the bioavailability of a drug in terms of ocular disease, the time that the drug stays on the cornea must be increased. There must be a set viscosity on the ocular formulations and a way to improve the viscosity is by increasing the amount of the oil face that is present in the nano-emulsion, thereby increasing the time that the drug settles on the cornea.
Liposomes
Liposomes are similar to nano-particles in its targeted drug delivery function. They consist of one or several concentric spheres which comprise of a lipid bilayer that is separated by aqueous or water compartments that are composed of phospholipids. They are able to encapsulate both hydrophobic as well as hydrophilic drug molecules, this quality helps liposomes perform as an ocular drug delivery system because it helps protect the drug molecule from any degradation from metabolic enzymes that are present on the surface of the eye as well as in the tear fluid.
Nanomicelles
Nanomicelles are nanosized colloidal suspensions that have a hydrophobic core and a hydrophilic shell. Rabbit animal model experiments on rapamycin nanomicellar eye drops revealed a noticeably higher concentration of the drug in the retina. These studies demonstrated that nanomicellar formulation enabled drug delivery to the posterior segment with topical eye drop formulation [11].
Nanotechnology-based drug delivery strategies for management of ocular disorders
Besides the current formulations such topical administration of antibiotics (eye drops), phototherapeutic surgery (PTK), transplantation of full thickness cornea (PK), nonsteroidal antiinflammatory drugs (NSAIDs), and steroids, novel nanotechnology-based drug delivery strategies for management of ocular disorders are coming up. Some of the evolving representative examples of nanotechnology-based drug delivery strategies for management of ocular disorders have been summarized in Table1.
| Table 1: Representative examples of nanotechnology-based drug delivery strategies for management of ocular disorders. | |||||
| Type of Formulation | Type of carrier polymeric Material & name of drug |
Size (nm) |
Applications/Functions | Remark | Ref |
| Nanoparticle | Polymer- Chitosan (Latanoprost acid: ocular hypotensive drug) |
200 |
|
Preclinical | [15] [26] |
| Nano wafer | Polymer-Poly (vinyl alcohol) (Axitinib: RTK Inhibitor) | 500 |
|
Preclinical | [15] [27] |
| Hydrogel | Polymer- Polyvinylpyrrolidone (Bevacizumab: a monoclonal antibody against VEGF-A) |
- |
|
Preclinical | [15] [16] [26] |
| Nanosusp ension | Polymer- MPEGPCL-VS block copolymer (Diclofenac: An antiinflammatory drug) |
105 |
|
Preclinical | [15] [17] [28] |
| Hydrogel (Virgan) |
Hydrophilic Polymer (Ganciclovir: a drug acute herpetic keratitis treatment) |
- |
|
Market | [15] [30] |
| Liposome | Polymer-Polyvinylpyrrolidone (Bevacizumab: a monoclonal antibody against VEGF-A) | 100- 200 |
|
Preclinical | [15] [18] [26] |
| Micelles | Polymer- Chitosan (Triamcinolone acetonide: a topical corticosteroid prescribed to relieve skin inflammation, itching, dryness, and redness) | 200- 350 |
|
Preclinical | [15] [19] [27] |
| Dendrimer | Polymer- PEG -coated cationic polymer (dendrimer-gene complex) | 50 |
|
Preclinical | [15] [20] [29] |
| Hydrogel | Polymer (Timoptic-XE) Timolol maleate |
- |
|
Market | [15] |
| Hydrogel | Polymer: Blend of Carbopol and Pluronic polymers |
|
Patented | [31] | |
The currently employed optical tools like Magnetic resonance imaging, Fundus photography, Ultrasonography, Optical coherence tomography, Confocal microscopy, Fluorescein angiography, Positron emission tomography etc. are mostly compatible for analysing the efficacy of nano-structured formulations against ocular disorders. Although, these techniques demonstrate huge promises, however, their progress in concert with nano-formulations is still in developing stage [21].
Advantages
Due to the extremely delicate features of the eye, as well as the eyes capacity to protect itself with multiple layers of biological barriers, it is often difficult for current drugs to pass through all the barriers or even the correct barriers in order to reach the targeted portion of the eye which can result in drug loss and low bioavailability. This is where nano-formulations have an advantage. Nano-formulations can minimize the precorneal drug loss caused by rapid tear fluid turnover. The size of the particle that carries the drug can also be adjusted according to the necessity (which barriers of the ocular system the drug needs to pass). Nano-formulations also pose less of a threat of toxicity, which in the case of ocular treatment is a large advantage.
Future prospectus of nano-formulations in ocular therapy
A decade before it was assumed that nano-formulations may not reach to clinical reality, but this turn out to be an illusion, as FDA has given approval for clinical usage of nano-formulations against variety of human diseases. For example, the first marketed ophthalmic nano-emulsion was developed in the early 2000’s and was approved by the FDA in 2002 for the delivery of 0.05% Cyclosporin A (Restasis®). Restasis® is a preservative-free anionic nano-emulsion. This nano-emulsion was used for the treatment of dry eye [23]. Cyclokat® is also a new nano-emulsion formulation of Cyclosporin A, which is currently in the market for the treatment of dry eye disease. The formulation is based on the Novasorb® technology developed by Novagali Pharma. This formulation uses novel cationic nano-emulsion methodology for drug delivery of topical nature. [24]. Recently, InSite Vision (USA) has formulated a new drug delivery medium called Durasite® (polycarbophil, edentate disodium dihydrate and sodium chloride), as a basis for an extensive range of ocular drugs. FDA approved a DuraSite formulation containing Besifloxacin to treat bacterial conjunctivitis (pink eye). The technology involves utilizing polycarbophil as a biodegradable matrix for holding drug microparticles for increased drug retention time [25].
Conclusion
The recent technology and innovations with nano-formulations have resulted in significant improvements in ocular disease therapy. As discussed earlier, as compared to traditional approaches of drug delivery, the nanotechnology based approaches have significantly helped in increasing drug bioavailability, the drug efficacy as well as there is significant decrease in the toxicity of nano-formulations when in comparison with the traditional therapeutic effects. Nano-formulations are able to be mass produced and can also be versatile in their morphology which significantly aids in the ability to adapt the nano-formations to the specific function that is needed. The growing number of preclinical and clinical studies and accumulating literature for the usage of nano-formulations in ocular therapy indicate that the nanotechnology based nano-formations and Nano-delivery settings might bring a paradigm shift in the management of ocular disorders.
References
- Ann-Marie Ako-Adounvo1, Ramesh C Nagarwal, Lais Oliveira, Sai H.S. Boddu, Xiang S Wang, et al. Recent patents on ophthalmic nanoformulations and therapeutic implications. Recent Pat Drug Deliv Formul. 2014; 8: 193-201. Ref.: https://goo.gl/cnNA1Y
- Carroll J, Neitz M, Hofer H, Neitz J, Williams DR. Functional photoreceptor loss revealed with adaptive optics: An alternate cause of color blindness. Proc Natl Acad Sci U S A. 2004; 101: 8461-8466. Ref.: https://goo.gl/Cm9RXU
- C.P Wilkinson, Frederick L Ferris, Ronald E Klein, Paul P Lee, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology J. 2003; 110: 1677-1682. Ref.: https://goo.gl/Ft5L3J
- Dyonne T Hartong, Eliot, L Berson, Thaddeus PD. Retinitis pigmentosa. The Lancet. 2006; 368: 18-24. Ref.: https://goo.gl/ErW6Yg
- Kenneth P Cheng, David A Hiles, Albert W Biglan, Milton C Pettapiece. Visual Results after Early Surgical Treatment of Unilateral Conenital Cataracts. Ophthalmology J. 1991; 98: 903-910. Ref.: https://goo.gl/X6RKJF
- SibelCetinel, Carlo Montemagno. Nanotechnology for the Prevention and Treatment of Cataract. Asia-Pacific J Ophthalmology. 2015; 4: 381-387. Ref.: https://goo.gl/74QdCK
- Jonathan L Haines, Michael A Hauser, Silke Schmidt, William K Scott, Lana M Olson, et al. Complement Factor H Variant Increases the Risk of Age-Related Macular Degeneration. Science Journal. 2005; 308: 419-421. Ref.: https://goo.gl/boQqiH
- Paul J Foster, Ralf Buhrmann, Harry A Quigley, Gordon J Johnson. The definition and classification of glaucoma in prevalence surveys. British J Opthamology. 2002; 86: 238-242. Ref.: https://goo.gl/HPTjnG
- Maurice DM, Mishima. Handbook of Experimental Pharmacology. In Ocular pharmacokinetics. 1989; 57: 16-119.
- Hong-Yang Zhou, Ji-Long Hao, Shuang Wang, Yu Zheng, Wen-Song Zhang. Nanoparticles in the ocular drug delivery. Int J Ophthalmol. 2013; 6: 390-396. Ref.: https://goo.gl/LatWrz
- Xiaoyong Yuan, Daniela C Marcano, Crystal S Shin, Xia Hua, Lucas C Isenhart, et al. Ocular Drug Delivery Nanowafer with Enhanced Therapeutic Efficacy. J American Chemical Society. 2015; 9: 1749-1758. Ref.: https://goo.gl/XUtyUL
- Bhatia S, Saurabh A. Natural Polymer Drug Delivery Systems. Springer International Publishing Switzerland. Natural Polymer Drug Delivery Systems. 2016; 1: 33-46.
- Noriaki Nagai, Yoshimasa Ito. A New Preparation Method for Ophthalmic Drug Nanoparticles. Pharm Anal Acta. 2014; 5: 305. Ref.: https://goo.gl/eLQZH7
- Shyam S Chaurasia, Rayne R Lim, Rajamani Lakshminarayanan, Rajiv R Mohan. Nanomedicine Approaches for Corneal Diseases. J Funct Biomater. 2015; 6: 277-298. Ref.: https://goo.gl/o7vjZs
- Yuhua Weng, Juan Liu, Shubin Jin, Weisheng Guo, Xingjie Liang et al. Nanotechnology-based strategies for treatment of Ocular disease. Acta Pharm Sin B. 2017; 7; 281-291. Ref.: https://goo.gl/xZzpFG
- Luu CD, Lau AM, Koh AH, Tan D. Multifocal electroretinogram in children on atropine treatment for myopia. British J Ophthalmol. 2005; 89: 151-153. Ref.: https://goo.gl/AMckhK
- Marzieh Fathi, Jaleh Barar, Ayuob Aghanejad, Yadollah Omidi. Hydrogels for ocular drug delivery and tissue engineering. Bioimpacts. 2015; 5: 159-164. Ref.: https://goo.gl/PZLm1j
- Vishal R Patel, Agrawal YK. Nanosuspension: An approach to enhance solubility of drugs. J Advanced Pharmaceutical Technology & Research. 2011; 2: 81-87. Ref.: https://goo.gl/hk6GWE
- Gyan P Mishra, Mahuya Bagui, Viral Tamboli, Ashim K Mitra. Recent Applications of Liposomes in Ophthalmic Drug Delivery. J Drug Delivery. 2011; 2011: 1-14. Ref.: https://goo.gl/P5EoBM
- Abhirup Mandal, Rohit Bisht, Ilva D Rupenthal, Ashim K Mitra. Polymeric micelles for ocular drug delivery: From structural frameworks to recent preclinical studies. J Controlled Release. 2017; 248: 96-116. Ref.: https://goo.gl/wXFVx4
- Ammar HO, Salama HA, Ghorab, Mahmoud. Nanoemulsion as a potential ophthalmic delivery system for dorzolamide hydrochloride. AAPS PharmSciTech. 2009; 10: 808-819. Ref.: https://goo.gl/Thnc6H
- Frederic Lallemand, Philippe Daull, Simon Benita, Ronald Buggage, Jean-Sebastien Garrigue. Successfully Improving Ocular Drug Delivery Using the Cationic Nanoemulsion, Novasorb. J Drug Delivery. 2012; 1-16. Ref.: https://goo.gl/A1kSiu
- Luigi Battaglia, Loredana Serpe, Federica Foglietta, Elisabetta Muntoni, Marina Gallarate, et al. Application of lipid nanoparticles to ocular drug delivery. Expert Opin Drug Deliv. 2016; 13: 1743-1757. Ref.: https://goo.gl/zYfRj1
- Marina Kalomiraki, Kyriaki Thermos, Nikos A Chaniotakis. Dendrimers as tunable vectors of drug delivery systems and biomedical and ocular applications. Int J Nanomedicine. 2016; 11: 1-12. Ref.: https://goo.gl/YC8TYi
- Harry A Quigley. Nanotechnology-based strategies for treatment of ocular disease. British J Opthamology. 1996; 7: 238-242.
- Yuan X, Marcano DC, Shin CS, Hua X, Isenhart LC, et al. Ocular drug delivery nanowafer with enhanced therapeutic efficacy. ACS Nano. 2015; 9: 1749-1758. Ref.: https://goo.gl/H4afK3
- Jiang M, Gan L, Zhu C, Dong Y, Liu J, et al. Cationic core shell lipo nanoparticles for ocular gene delivery. Biomaterials. 2012; 33: 7621-7630. Ref.: https://goo.gl/AYyRLF
- Shuai Shi, Zhaoliang Zhang, Zichao Luo, Jing Yu, Renlong Liang, et al. Chitosan grafted methoxy poly(ethylene glycol)-poly(ε-caprolactone) nanosuspension for ocular delivery of hydrophobic diclofenac. Sci Rep. 2015; 5: 11337. Ref.: https://goo.gl/3oZfgN
- Panagiotis Mastorakos, Siva P Kambhampati, Manoj K Mishra, Tony Wu, Eric Song, et al. Hydroxyl PAMAM dendrimer-based gene vectors for transgene delivery to human retinal pigment epithelial cells. Nanoscale. 2015; 7: 3845-3856. Ref.: https://goo.gl/N7Aqkg
- Colin J. Ganciclovir ophthalmic gel, 0.15%: a valuable tool for treating ocular herpes. Clin Ophthalmol. 2007; 1: 441-453. Ref.: https://goo.gl/2pkGU5
- Lin HR, Sung KC. Ophthalmic drug delivery formulations and method for preparing the same. 2003.