More Information
Submitted: February 17, 2023 | Approved: March 02, 2023 | Published: March 03, 2023
How to cite this article: Marconi V, Fortunato C, detto Rinaldini DM, Pascucci L, Arsego DM, et al. Hospital-acquired infections and antibiotic use in a geriatric hospital: a point prevalence study. Arch Pharm Pharma Sci. 2023; 7: 004-007.
DOI: 10.29328/journal.apps.1001037
Copyright License: © 2023 Marconi V, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Hospital-acquired infections and antibiotic use in a geriatric hospital: a point prevalence study
Vittorio Marconi1,2, Corinna Fortunato3 *, Davide Mengarelli detto Rinaldini3, Lidia Pascucci3, Daniele Arsego4 and Letizia Ferrara4
*, Davide Mengarelli detto Rinaldini3, Lidia Pascucci3, Daniele Arsego4 and Letizia Ferrara4
1Postgraduate School of Medical Statistics and Biometry, Department of Biomedical Sciences and Public Health, Marche Polytechnic University, 60126 Ancona, Italy
2Center of Epidemiology, Biostatistics and Medical Information Technology, Marche Polytechnic University, 60126 Ancona, Italy
3Department of Biomedical Sciences and Public Health, Section of Hygiene, Preventive Medicine and Public Health, Marche Polytechnic University, Ancona, Italy
4Italian National Research Centers on Ageing (INRCA-IRCCS), Ancona, Italy
*Address for Correspondence: Corinna Fortunato, Department of Biomedical Sciences and Public Health, Section of Hygiene, Preventive Medicine and Public Health, Marche Polytechnic University, Ancona, Italy, Email: [email protected]
Background: Healthcare-Associated Infections (HAIs) are the most common healthcare-associated complications, particularly in elderly patients. The aim of this study is to describe the prevalence of HAIs and associated risk factors in the IRCCS INRCA of Ancona.
Methods: A cross-sectional study has been carried out. Data has been collected in accordance with the European Centre for Disease Prevention and Control (ECDC) Point Prevalence Survey 2022-2023 (PPS3) protocol in the IRCCS INRCA of Ancona in November 2022.
Results: Out of the 128 patients included in our study, 75.0% were over 78 years old and 9.1% presented an active HAI on the day of the survey. The prevalence of HAIs varied based on the length of the hospital stay (OR 1.1, CI 95% 1.05 - 1.17, p < 0.001) and hospitalization > 7 days (OR 5.9, CI 95% 1.2 - 28.7, p = 0.02).
Conclusion: It is clear from our findings that HAIs are associated with advanced patient age, prolonged hospital stay, and use of medical devices, especially in those patients that, due to their clinical situation, are more vulnerable. Although some of these infections can easily be treated, it is important to develop effective infection control strategies thanks to antimicrobial stewardship programs.
Healthcare-Associated Infections (HAIs) are the most common healthcare-associated complications. These infections considerably increase the costs of healthcare and are detrimental to patients’ health [1].
The Centre for Disease Control and Prevention (CDC) identifies that nearly 1.7 million hospitalized patients each year acquire HAIs while being treated for other health problems and that more than 98,000 of these patients (1 in 17) die as a result of these infections [1].
According to the European Centre for Disease Prevention and Control (ECDC) which analyzed a total of 310,755 patients in 1,209 hospitals from 28 European Countries, 6.5% of patients were affected by an HAI and a total of 8.9 million estimated episodes per year [2].
Enterobacteriaceae, Acinetobacter baannii, Pseudomonas aeruginosa, Staphylococcus aureus, Clostridium difficile and enterococci were the most frequently isolated microorganisms in European Hospitals [2]. Antibiotics are one of the most prescribed drug classes, yet the incidence of inappropriate antibiotic prescription (molecule, duration, or dosage) remains high [3]. Their incorrect use leads to the progressive selection of multidrug-resistant microorganisms with an epidemiological and economic impact, exacerbated by the rapid loss of efficacy of an increasing number of antibiotics and the reduced development of new antibiotic molecules over the past decade [4,5].
The World Health Organization Health Organization (WHO) considers this problem one of the three most important public health threats of the 21st century, along with the climate crisis and the trend toward vaccine rejection [6].
Italians aged ≥ 65 years in 2021 constituted 23.5% of the Italian population, but by 2050 it is estimated that this proportion will increase to 34.9% [7]. As patients age, the phenomenon of immunosenescence leads to increased risk of morbidity and mortality secondary to infectious disease processes due to a decline in both quantitative and qualitative immune function [8]. The aim of this study is to describe the prevalence of HAIs and associated risk factors and the use of antibiotics in the IRCCS INRCA Italian National Research Centers on Ageing of Ancona.
The study was conducted in November 2022 in the IRCCS INRCA of Ancona, according to the Point Prevalence Survey 3 protocol proposed by the ECDC. All patients admitted to the wards at or before 8 a.m. and not discharged at the time of the survey have been included.
Data collection for each department was completed in a single day, using the electronic medical record.
An active healthcare-associated infection (associated with acute care hospital stay) present on the day of the survey is defined as an active infection is active if signs and symptoms of the infection are present on the survey date or signs and symptoms were present in the past and the patient is (still) receiving treatment for that infection on the survey date. The presence of symptoms and signs should be verified until the start of the treatment in order to determine whether the treated infection matches one of the case definitions of healthcare-associated infection and the onset of symptoms was on Day 3 or later (day of admission = Day 1) of the current admission; or the patient presents with an infection but has been readmitted fewer than 48 hours after a previous discharge or transfer from a healthcare facility; or the patient has been admitted (or develops symptoms within two days) with an infection that meets the case definition of an active surgical site infection (SSI), i.e. the SSI occurred within 30 days of the operation (or in the case of surgery involving an implant, was a deep or organ/space SSI that developed within 90 days of the operation) and the patient either has symptoms that meet the case definition and/or is on antimicrobial treatment for that infection; or the patient has been admitted (or develops symptoms within two days) with C. difficile infection fewer than 28 days after a previous discharge or transfer from a healthcare facility; or an invasive device was placed on Day 1 or Day 2, resulting in an HAI before Day 3; or onset of symptoms on Day 1 or Day 2 in a newborn; or the patient was diagnosed with COVID-19 and the onset of symptoms (or first positive test if asymptomatic) was on Day 3 or later (day of admission = Day 1) of the current admission or the patient has COVID-19 on admission (or onset before Day 3) and was (re-)admitted fewer than 48 hours after a stay of more than seven days in the same or another healthcare facility [9]
In total, 132 cases were analyzed and four patients were excluded from the study because the HAIs were related to another care facility [10].
The survey protocol was approved by the ethics committee of the Università degli Studi di Torino (Prot. No. 0421518 of 29/07/2022).
Any information relating to a patient participating in the surveillance was collected and treated in pseudonymized form, while the research results are made available through scientific publications anonymously, carefully, and rigorously avoiding any detail that could in some way allow third parties to trace their identity. Furthermore, the data is retained in compliance with current legislation on the processing of personal data (EU Regulation No. 2016/679, D.lgs.196/2003 amended by D.lgs.101/2018) by the Data Controller identified in the Istituto Superiore di Sanità (ISS).
Of the 128 patients included, 56.3% (72) were female, 75.0% (96) were over 78 years old and 9.1% (12) had a Healthcare-Acquired Infection on the day of the survey.
The area of care with the most infections is the medical area where 53.9% are located, followed by the surgical area (25.0%) and post-acute care (21.1%) Table 1.
| Table 1: Characteristics of patients enrolled at the time of the survey. | ||||||
| All patients (n = 128) | With HAI (n = 12) |
Without HAI (n = 116) | ||||
| Gender | ||||||
| Male | 57 | 44.5% | 4 | 33.3% | 53 | 55.7% |
| Female | 71 | 55.5% | 8 | 66.7% | 63 | 54.3% |
| Age | ||||||
| 0-77 | 32 | 25.0% | 1 | 8.3% | 31 | 26.7% |
| 78-84 | 28 | 21.9% | 2 | 16.7% | 26 | 22.4% |
| 85-89 | 34 | 26.6% | 3 | 25.0% | 31 | 26.7% |
| > 89 | 34 | 26.6% | 6 | 50.0% | 28 | 24.1% |
| Field | ||||||
| Medicine | 69 | 53.9% | 6 | 50.0% | 63 | 54.3% |
| Surgery | 32 | 25.0% | 4 | 33.3% | 28 | 24.1% |
| Post-Acute Care | 27 | 21.1% | 2 | 16.7% | 25 | 21.6% |
| Devices | ||||||
| CVC | 16 | 12.5% | 1 | 8.3% | 15 | 12.9% |
| Urinary catheter | 66 | 51.6% | 9 | 33.3% | 57 | 49.1% |
| Surgery | ||||||
| NHSN | 6 | 4.7% | 1 | 8.3% | 5 | 4.3% |
| Minimally invasive | 26 | 20.3% | 4 | 33.3% | 22 | 19.0% |
| Hospitalization, median | 7 | (4-14) | 20 | (17-32) | 7 | (4-12) |
At univariate analysis (Student’s t, Mann-Whitney), three characteristics were identified that show a statistically significant difference between the groups of patients with HAI and without (p < 0.1): age of the patient, presence of urinary catheter and length of hospital stay (from time of admission to time of detection).
A multivariate analysis (logistic regression) was then conducted to calculate the odds ratio (OR) and confidence interval (CI), using the factors noted: duration of hospitalization (OR 1.1, CI95% 1.05 - 1.17, p < 0.001) and hospitalization > 7 days (OR 5.9, CI 95% 1.2 - 28.7, p = 0.02) Table 2.
| Table 2: Length of hospital stay of patients with HAI. | ||||
| Patients with HAI | ||||
| Length of hospital stay | n | OR | CI95% | p |
| ≤ 7 days | 2 | - | - | - |
| > 7 days | 10 | 5.9 | 1.2 - 28.7 | 0.02 |
| Total | 12 | |||
Urinary tract infections (n = 4) were the most frequent HAIs, of which one was sustained by Morganella Morganii and another one by Klebsiella Pneumoniae Carbapenemase (KPC), followed by three SARS-CoV-2 infections (25.0% of HAI), two pneumoniae (16.7% of HAIs), two skin and soft tissue infections (16.7% of HAI), of which one sustained by Escherichia Coli and one Clostridium Difficile gastrointestinal infection (8.3% of HAI) Table 3.
| Table 3: Prevalence distribution of major HAI by location. | ||
| Types of infection | n | % of HAI |
| UTIs | 4 | 33.3 |
| Pneumoniae | 2 | 16.7 |
| Skin and soft tissue Infections | 2 | 16.7 |
| Gastrointestinal Infections | 1 | 8.3 |
| COVID19 Infections | 3 | 25.0 |
| Total | 12 | |
Almost half of the patients (45.3%) were on antibiotics on the day of the survey but in 10.3% of cases, the reason for treatment was not motivated in the clinical chart. Surgery prophylaxis accounted for 17.2% of antibiotic therapies and in half of these cases it lasted for at least two days.
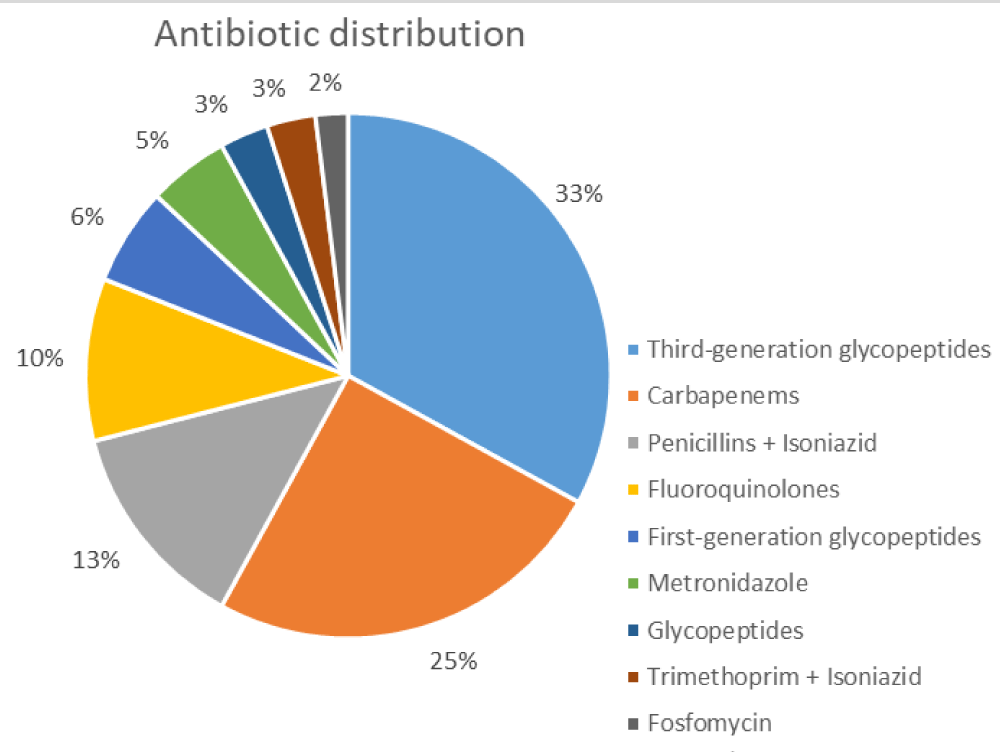
The most widely administered class of antibiotics is third-generation cephalosporins, followed by carbapenems and penicillins with isoniazid Figure 1.
Figure 1: Prevalence distribution of major classes of antibiotics.
Our findings show that the most relevant risk factors for HAIs are advanced patient age, prolonged hospital stay, and use of medical devices, as already documented in previous studies [11,12].
In particular, a hospital stays longer than 7 days represents the element most strongly associated with HAIs (OR 5.9; p = 0.02).
It is clear that it is not always possible to reduce the length of hospitalization (e.g., post-acute care, rehabilitation) and this is particularly true for elderly patients, like those of our study sample; however, there is room for improvement.
HAIs prevalence studies are very useful Hospital Hygiene tools that should be performed periodically, in conjunction with a laboratory monitoring system of multiresistant/alert microorganisms and an antimicrobial stewardship program [13].
Moreover, making HAIs data publicly available is fundamental to enhancing the knowledge of microorganisms’ circulation and their patterns of resistance so that actions can be taken [14].
- Haque M, Sartelli M, McKimm J, Abu Bakar M. Health care-associated infections - an overview. Infect Drug Resist. 2018 Nov 15;11:2321-2333. doi: 10.2147/IDR.S177247. PMID: 30532565; PMCID: PMC6245375.
- Suetens C, Latour K, Kärki T, Ricchizzi E, Kinross P, Moro ML, Jans B, Hopkins S, Hansen S, Lyytikäinen O, Reilly J, Deptula A, Zingg W, Plachouras D, Monnet DL; Healthcare-Associated Infections Prevalence Study Group. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Euro Surveill. 2018 Nov;23(46):1800516. doi: 10.2807/1560-7917.ES.2018.23.46.1800516. Erratum in: Euro Surveill. 2018 Nov;23(47): PMID: 30458912; PMCID: PMC6247459.
- Versporten A, Zarb P, Caniaux I, Gros MF, Drapier N, Miller M, Jarlier V, Nathwani D, Goossens H; Global-PPS network. Antimicrobial consumption and resistance in adult hospital inpatients in 53 countries: results of an internet-based global point prevalence survey. Lancet Glob Health. 2018 Jun;6(6):e619-e629. doi: 10.1016/S2214-109X(18)30186-4. Epub 2018 Apr 23. Erratum in: Lancet Glob Health. 2018 Sep;6(9):e968. PMID: 29681513.
- Christaki E, Marcou M, Tofarides A. Antimicrobial Resistance in Bacteria: Mechanisms, Evolution, and Persistence. J Mol Evol. 2020 Jan;88(1):26-40. doi: 10.1007/s00239-019-09914-3. Epub 2019 Oct 28. PMID: 31659373.
- Vandael E, Latour K, Goossens H, Magerman K, Drapier N, Catry B, Versporten A; Belgian Point Prevalence Survey Study Group. Point prevalence survey of antimicrobial use and healthcare-associated infections in Belgian acute care hospitals: results of the Global-PPS and ECDC-PPS 2017. Antimicrob Resist Infect Control. 2020 Jan 13;9(1):13. doi: 10.1186/s13756-019-0663-7. PMID: 31956402; PMCID: PMC6958935.
- World Health Organization. Global action plan on antimicrobial resistance. World Health Organization. 2015. https://apps.who.int/iris/handle/10665/193736
- ISTAT (2022) - Previsioni della popolazione residente e delle famiglie - https://www.istat.it/it/files//2022/09/REPORT-PREVISIONI-DEMOGRAFICHE-2021.pdf
- Giarratano A, Green SE, Nicolau DP. Review of antimicrobial use and considerations in the elderly population. Clin Interv Aging. 2018 Apr 17;13:657-667. doi: 10.2147/CIA.S133640. PMID: 29713150; PMCID: PMC5909780.
- Point prevalence survey of healthcare-associated infections and antimicrobial use in European acute care hospitals. Protocol version 6.1, ECDC PPS 2022-2023. https://www.ecdc.europa.eu/sites/default/files/documents/antimicrobial-use-healthcare-associated-infections-point-prevalence-survey-version6-1.pdf
- Russo Fiorino G, Maniglia M, Marchese V, Aprea L, Torregrossa MV, Campisi F, Favaro D, Calamusa G, Amodio E. Healthcare-associated infections over an eight year period in a large university hospital in Sicily (Italy, 2011-2018). J Infect Prev. 2021 Sep;22(5):220-230. doi: 10.1177/17571774211012448. Epub 2021 Jun 22. PMID: 34659460; PMCID: PMC8512876.
- Wolkewitz M, Schumacher M, Rücker G, Harbarth S, Beyersmann J. Estimands to quantify prolonged hospital stay associated with nosocomial infections. BMC Med Res Methodol. 2019 May 31;19(1):111. doi: 10.1186/s12874-019-0752-6. PMID: 31151418; PMCID: PMC6544970.
- Ssekitoleko RT, Oshabaheebwa S, Munabi IG, Tusabe MS, Namayega C, Ngabirano BA, Matovu B, Mugaga J, Reichert WM, Joloba ML. The role of medical equipment in the spread of nosocomial infections: a cross-sectional study in four tertiary public health facilities in Uganda. BMC Public Health. 2020 Oct 16;20(1):1561. doi: 10.1186/s12889-020-09662-w. PMID: 33066745; PMCID: PMC7562759.
- Sharif M, Aslam S, Saleem Z. Point prevalence survey to estimate antimicrobial use in a tertiary care university hospital in Pakistan using WHO methodology: findings and implications. Infect Dis (Lond). 2022 Sep;54(9):698-701. doi: 10.1080/23744235.2022.2064544. Epub 2022 Apr 19. PMID: 35439103.
- Maurici M, D'Alò GL, Fontana C, Santoro V, Gaziano R, Ciotti M, Cicciarella Modica D, De Filippis P, Sarmati L, De Carolis G, Pica F. Microbiology and Clinical Outcome of Hospital-Acquired Respiratory Infections in an Italian Teaching Hospital: A Retrospective Study. Healthcare (Basel). 2022 Nov 12;10(11):2271. doi: 10.3390/healthcare10112271. PMID: 36421594; PMCID: PMC9691183.