More Information
Submitted: June 24, 2024 | Approved: July 03, 2024 | Published: July 04, 2024
How to cite this article: Ofomata CM, Ezeama NN, Ezejiogu C. Experiences of Consumers on the Health Effects of Fake and Adulterated Medicines in Nigeria. Arch Pharm Pharma Sci. 2024; 8(1): 075 - 081.
DOI: 10.29328/journal.apps.1001059
Copyright License: © 2024 Ofomata CM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction inany medium, provided the original work is properly cited.
Keywords: Fake and adulterated medicines; Globalization
Experiences of Consumers on the Health Effects of Fake and Adulterated Medicines in Nigeria
Chijioke M Ofomata1, Chijioke M Ofomata2 and Chinelo Ezejiogu3*
1Department of Forensic Sciences, Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University, Agulu, Awka, P.M.B 5025, Anambra State, Nigeria
2Department of Community Medicine and Primary Healthcare, Faculty of Medicine, College of Health Sciences, Nnamdi Azikiwe University, Awka, Nigeria
3Department of Pharmaceutical Microbiology, Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University, Awka, Anambra State, Nigeria
*Address for Correspondence: Chinelo Ezejiogu, Department of Pharmaceutical Microbiology, Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University, Awka, Anambra State, Nigeria, Email: [email protected]
Medicines are used to cure and treat ailments, relieve or eliminate disease symptoms, and slow down the disease process. Any attempt to disrupt this natural medicine process, using falsified medications, spells doom to a consumer of such medication. The challenge of fake medicines is a global one and affects developing and developed nations and currently assumes great significance as a result of globalization challenges, which have flattened the entire world, hence removing barriers to the movement of products and services. The cross-sectional survey was conducted, using six local government areas of Anambra State in South-East Nigeria, namely Awka, Nnewi, Onitsha, Aguata, Ogbaru, and Anaocha, among adults aged 18 years and above. A minimum sample size of 500 was calculated and stratified sampling was employed to select respondents in order to ensure that various population groups, the upper class, middle class, and lower class were represented.
This research has shown that falsified medicine is an evil wind that blows nobody any good. It negatively affects every aspect of the citizen’s livelihood, ranging from their health, which manifests as treatment failures, deformities, loss of life to death, to loss of confidence in the healthcare providers, revenue losses to individuals, healthcare providers, manufacturers, and finally corruption of the genuine medicines supply chain with fake and adulterated medicines.
The study has clearly shown the experiences of residents of Anambra State, South-East Nigeria with fake and adulterated medicines and also services as a wake-up call to medicines regulators like NAFDAC, PCN, the PSN, and Federal Ministry of Health to declare a state of emergency on the fight against fake and adulterated medicines and make enabling laws that are punitive enough towards the fight against this scourge, so that the healthcare and well-being of Nigerians would be assured at all times.
A major challenge faced by populations of developing nations is poor access to life-saving medicines, however, an even worse challenge is the occurrence of fake medications. A significant number of impoverished and low-income countries in sub-Saharan Africa lack the resourcefulness to manage the menace posed by fake medicament in society. This contributes to the present burden of poverty, ill health, lack of basic infrastructure, conflicts and wars, and other adversities experienced in these countries [1].
The World Health Organisation estimates that about 10% of medicaments moving globally and 25% in developing nations are fake. Some parts of Asia and Africa are the worst affected, followed closely by Latin America [2]. Almost every category of medicament is being faked, including antibiotics, anticancer agents, and endocrine drugs [3]. Developing countries faced with a heavy burden of communicable diseases find that their range of fake medicaments are principally antibiotics, unlike developed countries, where drugs used to treat chronic diseases such as cancer medication, lipid-lowering drugs, and lifestyle drugs, anti-allergic and endocrine medication (example, hormones, and steroids) and also drugs for the treatment of erectile dysfunction dominate the fake medications market [4,5].
The use of fake medications causes grave harm to patients’ health such as adverse drug reactions and even death [6]. It can result in drug resistance which can lead to treatment failure as well as negatively affect patients’ response to genuine medication in the future, even in patients who have not used fake medicines [7,8]. It has been estimated that about 100,000 Africans die annually from the usage of fake medications. Furthermore, about 200,000 deaths per year could be averted if illnesses are treated with standardized medicines [9,10]. Media reports abound of the grievous impact of fake and adulterated medications. For example, in Nigeria in 1990 and in Haiti in 1995, about one hundred children in both countries died following ingestion of cough syrup contaminated with diethylene glycol (antifreeze) [11,12]. Eighty-four children also died in Nigeria between late 2008 and early 2009 following consumption of a teething medicine, ‘My Pikin Baby Teething Mixture’, distributed by the NAFDAC-licensed Barewa Pharmaceuticals, also contaminated with diethylene glycol [13-17]. Similar horror stories have been reported in China (Goodman, 2002) and Niger Republic [18,19].
Patients, consumers/buyers of pharmaceuticals are vulnerable to the effects of fake and adulterated medications but may be unaware of the quality of the products they are purchasing [20]. Furthermore, geographical accessibility, shorter waiting times, longer opening hours, greater confidentiality, more personable social interaction, ease of seeking advice, lower costs, flexible pricing policies, and no separate consultation fee are some of the reasons why consumers may patronise drug peddlers rather than registered pharmacies. Unfortunately, one of the challenges that characterise the self-medication of drugs from drug peddlers is that in most cases, neither the drug seller nor the consumer is aware of the correct dosage and duration of treatment [21]. The effects of fake and adulterated medicine have been under-reported, particularly in under-developed nations, because end users do not associate often therapeutic failure with fake medications, but may attribute it to other factors such as contamination of drinking water supply, disease complications, lack of proper feeding, failure to complete the course of treatment or even a belief in curses or witchcraft [22].
This study, therefore, aims to assess the experiences of consumers of medicines on the health effects of fake, adulterated, and falsified medicines in Nigeria, using Anambra State as a case study.
This was a cross-sectional survey. The study was conducted in six local government areas in Anambra state, south-eastern Nigeria, namely Awka, Nnewi, Onitsha, Aguata, Ogbaru, and Anaocha. The study population comprised adults aged 18 years and older residing. A minimum sample size of 500 was calculated and stratified sampling was employed to select respondents in order to ensure that various population groups, the upper class, middle class, and lower class were represented. A semi-structured questionnaire was self-administered to the respondents after obtaining their consent. Data collected was analysed using Statistical Package for the Social Sciences (SPSS) version 25. Frequency distributions and proportions of the variables of interest were calculated and presented here using tables and charts.
A total of 500 questionnaires were distributed and 449 were returned, giving a response rate of 89.8%.
The socio-demographic characteristics of the respondents are shown in Table 1. Respondents in the 21-35 years age group were in the majority (73.5%). There were 216 females (48.1%) and 191 males (42.5%); 42 (9.4%) did not indicate their sex. The majority (79.2%) had an undergraduate degree/certificate while 20.8% had a post-graduate degree; 65 (14.5%) did not report their educational level. Regarding the source of medications, 75 (16.7%) respondents sourced their drugs from patent medicine shops, followed by pharmacy outlets (43 respondents; 9.6%), drug shops in open markets (33 respondents; 7.3%), people who hawk medicines on the bus (25 respondents; 5.6%), and on the streets (24 respondents; 5.3%).
| Table 1: Sociodemographic characteristics of respondent’s ways to curb fake and adulterated medicines in Nigeria. | ||
| Variable | Frequency | Percentage |
| Age of respondents (years) (n = 396) | ||
| 21-35 | 291 | 73.5 |
| 36-45 | 44 | 11.1 |
| 46 and older | 61 | 15.4 |
| Sex of respondents (n = 407) | ||
| Female | 216 | 53.1 |
| Male | 191 | 46.9 |
| Highest level of education (n = 384) | ||
| First degree, ND, NCE, HND | 304 | 79.2 |
| Masters, PhD and above | 80 | 20.8 |
| Source of medications (n = 449, multiple responses) | ||
| Hospitals and clinics | 18 | 4 |
| Pharmacy outlets | 43 | 9.6 |
| Patent medicine shop | 75 | 16.7 |
| Street drug hawkers | 24 | 5.3 |
| Bus drug hawkers | 25 | 5.6 |
| Drug shop in open markets | 33 | 7.3 |
| Nursing homes | 3 | 0.7 |
| Avoid self-medication, patronising of touts | 174 | 47.8 |
Table 2 summarises the respondents’ perceptions of their experiences regarding fake and adulterated medicines. 92% of valid respondents said that they have been personal victims of falsified medicines, as against the 8% that have never been victims. 17.9% of valid respondents agreed that someone close to them had been killed by falsified medicines while 82.1% had no such experience. When asked whether they knew anyone maimed by fake and adulterated medicines, 48 (14.5%) of valid respondents answered in the affirmative, and 284 respondents (85.5%) answered in the negative.
| Table 2: Experiences of respondents regarding use of fake and adulterated medicines | ||
| Variable | Frequency | Percentage |
| I am a personal victim of fake medicines (n = 163) | ||
| Yes | 150 | 92 |
| No | 13 | 8 |
| Fake medicines has killed somebody close to me (n = 341) | ||
| Yes | 61 | 82.1 |
| No | 280 | 17.9 |
| Fake medicines has maimed someone I know (n = 332) | ||
| Yes | 48 | 14.5 |
| No | 284 | 85.5 |
| I have been hospitalized as result of fake medicines (n = 330) | ||
| Yes | 98 | 29.7 |
| No | 232 | 70.3 |
| I have had medical complications due to the intake of fake medicines (n = 330) | ||
| Yes | 18 | 4 |
| No | 312 | 96 |
| Fake medicines caused my delayed recovery from sickness (n = 332) | ||
| Yes | 205 | 61.7 |
| No | 127 | 38.3 |
| Fake drugs have reduced my confidence in health care providers (n = 343) | ||
| Yes | 190 | 55.4 |
| No | 153 | 44.6 |
Furthermore, 98 (29.7%) of the respondents confirmed that they had been hospitalized due to fake and adulterated medicines whereas 232 (70.3%) of valid respondents said that they had never been hospitalized as a result of fake and adulterated medicines. Eighteen respondents (4.0%) had experienced medical complications as a result of the use of fake and adulterated medicines as opposed to 312 (94.8%) valid respondents who said that they had not.
Table 3 describes the respondents’ perceptions of the factors that enable the distribution of fake and adulterated medicines in Nigeria. About two-thirds (65%) were of the opinion that being able to obtain any type of prescription medication or injectable from patent medicine shops enabled the occurrence of fake and adulterated medicines in the country. The majority of the respondents (94.6%) agreed that open drug markets harbouring fake drug merchants were an enabling factor. Other factors assessed include their perceptions on the possible existence of a trans-national syndicate of wealthy and influential people controlling the fake drug market (80% agreed this was an enabling factor), that one does not require any qualifications in order to sell medicine (71.4% agreed to this) among others.
| Table 3: Respondents’ perceptions of factors that enable the distribution of fake and adulterated medicines in Nigeria. | ||
| Variable | Frequency | Percentage |
| Any prescription drug or injectable can be bought from patent medicine shops (n = 389) | ||
| Agree | 253 | 65 |
| Disagree | 136 | 35 |
| Medicines are sold like any other article of trade in open markets in Nigeria | ||
| Agree | 302 | 78 |
| Disagree | 85 | 22 |
| Anybody can sell medicines in Nigeria, whether qualified or not (n = 392) | ||
| Agree | 280 | 71.4 |
| Disagree | 112 | 28.6 |
| The fake drugs market is controlled by a trans-national syndicate of wealthy and influential people (n = 372) | ||
| Agree | 300 | 80.6 |
| Disagree | 72 | 19.4 |
| Chaotic drug distribution encourages fake drugs in Nigeria (n = 371) | ||
| Agree | 334 | 90 |
| Disagree | 37 | 10 |
| Open drug markets harbour fake drug merchants (n = 392) | ||
| Agree | 371 | 94.6 |
| Disagree | 21 | 5.4 |
| The punishment for falsifying drugs in Nigeria is too light (n = 376) | ||
| Agree | 333 | 88.6 |
| Disagree | 43 | 11.4 |
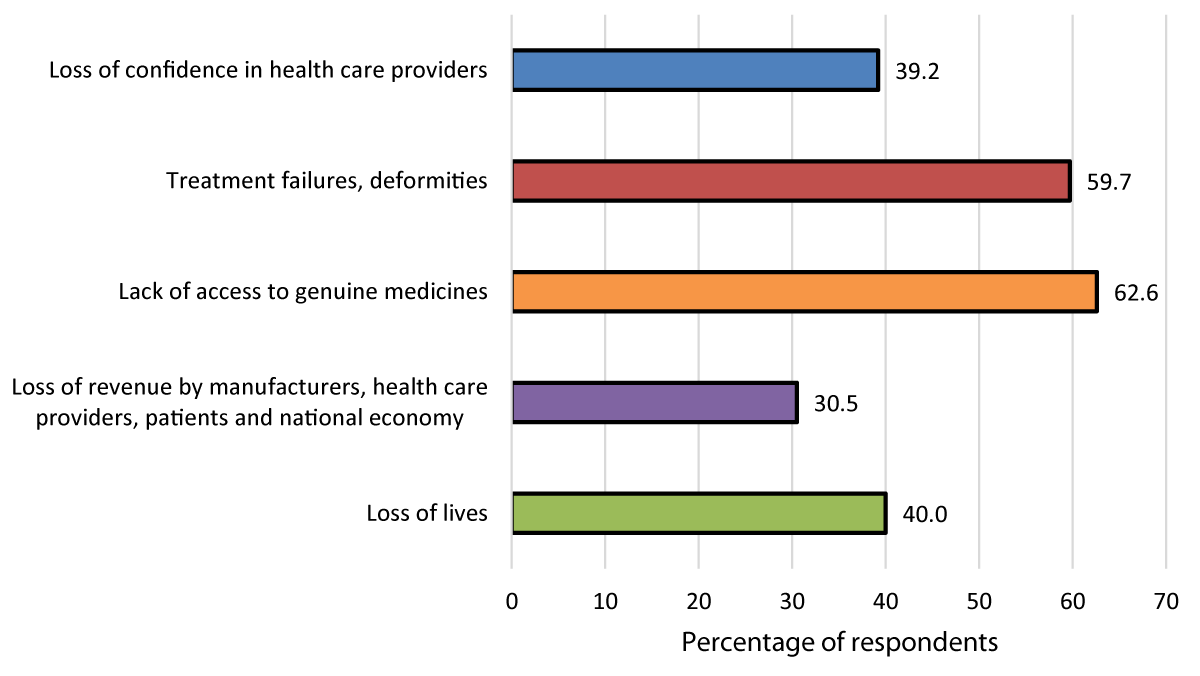
In Figure 1, the perceptions of respondents on the direct impact of fake and adulterated medicines are presented. The most frequent response was that the distribution of fake and adulterated medicines reduced access of the population to genuine medications (62.6% of respondents) while the least frequent response was that fake and adulterated medicines lead to losses of revenue by manufacturers, healthcare providers, patients and national economy (30.5%. of the respondents).
Figure 1: Perceptions of respondents on the direct impact of fake and adulterated medicines.
When the respondents were asked to suggest ways to curb the problem of fake and adulterated medicines in Nigeria, the most frequent answers among the range of responses included the Nigeria government declaring a state of emergency on fake and adulterated medicine (84.7%), patients/consumers avoiding self-medication and patronising of touts (47.8%), reporting suspects to the authorities (35.4%) and so on. These are shown in Table 4.
| Table 4: Respondents’ suggestions (n = 364). | ||
| Variable | Frequency | Percentage |
| Obey existing laws on safe medication (n = 364) | 23 | 6.3 |
| Be ambassadors against fake and adulterated medicine (n = 364) | 38 | 10.4 |
| Report suspects to the authorities (n = 364) | 129 | 35.4 |
| Government should declare a state of emergency on fake and adulterated medicines (n = 398) | 337 | 84.7 |
The results of this study show that the most frequent source of purchased medications, whether prescription-only or over-the-counter (OTC) medications, were patent medicines shops. Patent medicines shops and hawkers offer these products at lower rates than professionals in Pharmacies and hospitals, who charge a small premium on their cost as a result of their overhead and professional services [23].
Olike Chinwendu [24] in her paper, “The fight against fake drugs by NFDAC, in Nigeria” categorised these people as informal drug sellers, who sell medicines in an unregulated manner, without professional services, and with little knowledge of Pharmacy and Pharmacy practice. She went further to say that their only objective is to make a profit no matter whose ox is gored. They are on our streets as patent medicines dealers, street drug hawkers, hawkers in motor parks, buses, and sellers in open drug markets. She concluded by saying that this chaotic drug distribution by these non-professionals worsens the incidence of fake and adulterated medicines in Nigeria. Prazuck, et al. [25] opined that in many developing nations, medicine sellers show a lack of concern for expiration dates and storage conditions, especially in poor settings and in the absence of national control, and this increases the spread of sub-standard medicines.
An underlying contributory factor is the high poverty level in Nigeria which may compel citizens to seek cheaper and affordable medicines [26]. Due to the fact that a greater percentage of Nigerians are very highly impoverished and living below the poverty line, at an average GDP of less than one USD ($1) per day, most of them on taking ill, refuse to seek doctors’ attention or go to the nearest pharmacy for medical attention, but will first of all seek for alternative way of getting healing, namely, prayers, herbs and finally if these are not positive, he will then approach a patent medicine man with the instruction to give just a dose of the product, whether he is infected or suffering from malaria does not matter to him but all he knows is that he wants to get well but does not have enough money to get the full dosage of the product. This makes him ask for something that will alleviate his symptoms to enable him to still go to work and put food on his family’s table at least once a day. The economic hardship on Nigerians has affected to a large extent their preference for patronizing the patent medicines vendors. When asked why, he will politely let you know that he is aware that the patent man is not the best for himself and his family but that he simply cannot afford the luxury of visiting either a pharmacy or a hospital.
In Nigeria, we still operate the out-of-the-pocket financing option in our health systems financing, unlike other nations of the world that allow financial resources to follow their healthcare by using the financing option that allows the rich to pay more so as to subsidize the health bills of the poor fellow down the street [23]. When their health deteriorates, that means that anything can happen as neither the government nor individuals, not even those who stole their common resources, will come to their assistance, thereby leaving them vulnerable to the cold arms of death [23].
The economic situation of most Nigerians further empowers the patent medicines man and the hawker on the street, as they meet the so-called needs of the masses. Hence the patent medicines dealers and hawkers grow stronger and stronger, as they have ready customers for their illicit products and practice. Hence fake drugs are encouraged in our society through these patent medicines dealers whose objective is to make a profit at all times and in all circumstances no matter whose ox is gored.
This agrees with the literature on one of the reasons why fake and adulterated medicines are prevalent in Nigerian and third-world countries. Erhun, Babalola, and Erhun [26] submitted that reasons for the continued existence and increase in the rate of fake drugs differ from region to region according to the political, economic, and social-cultural characteristics of those nations. They went ahead to say that for highly impoverished nations like Nigeria, demand for affordable essential medicines is very high with about 70% of the medicines imported and distributed chaotically through various existing channels and the majority of the population purchasing their medicines from open markets, patent medicines and medicines hawkers in motor parks, buses and streets, irrespective of the kind of medicines they want to buy prescription only, OTC, and other lifesaving medicines.
This study examined the factors that enable the distribution of fake and adulterated medicines in Nigeria, from the perspective of the respondents. A most frequent opinion was that medicines are sold like any article of trade in open markets and under extreme temperatures and storage conditions, which are highly unsafe for medicines. The open markets are scattered all over the six geopolitical zones of the country and the patent shops are located at every nook and cranny of the country, all being manned by illiterates who did some years of apprentice program with their masters who sell drugs either in the markets or on the streets [23].
The chaotic distribution of medicines in Nigeria goes a long way to encouraging the faking of medicines by these illiterate drug traders in order to make money and be recognized in a society, like ours, that worships money, despite its source [23].
The respondents agreed with the fact that the peddling of fake medicines in Nigeria is engineered and controlled by a transnational syndicate of wealthy and influential people. Transnational trade in fake and adulterated medicines is a major challenge at Nigeria ports of entry, where some drug importers in a bid to evade inspection and detection make false entries and declarations about the nature or content of products in their containers, and hence employ unimaginable concealment strategies to cover their illegal importation activities. In 2003, a large consignment of a controlled narcotic analgesic was hidden in T-shirt packs and imported from India through Lagos airport. In 2004, 32 containers of various pharmaceuticals were imported and manifested as motor vehicle spare parts. They were moved to various locations within the ports to avoid detection. NAFDAC inspectors have also found drugs concealed in the inner part of containers containing textiles, candles, and shoes [27]. Pharmaceutical trade in cyberspace makes it even more difficult to tackle rogue online pharmacies is that they are more resilient to national legislations and more difficult to track than conventional pharmaceutical crimes, given their evanescent, transnational, and anonymised nature [28].
The majority of the respondents had been victims of fake medications. Some had experienced the death of someone close to them or had been hospitalized as a result of using fake medication. The use of falsified medications can result in treatment failures [29] and can seriously damage a patient’s health or even cause death [30]. Falsified medicines create uncertainty, confusion, and doubts about the value of the real drug and may lead to the use of alternative, less-desirable medicines or interventions [31]. They not only snatch income from consumers, by having them pay for products that have little or no therapeutic value, but they also lead to unresolved health challenges, and ultimately death [32].
The respondents’ perceptions on the direct impact of fake and adulterated medications show that these medicines are an evil wind that blows nobody any good, as it affects every aspect of our livelihood, from patients losing confidence in the healthcare workers, revenue losses by the manufacturers, healthcare providers, the patients and the nation at large, the citizen’s health being affected by treatment failures and deformities, losing of citizens to death and finally corruption of the genuine medicines supply chain with fake and adulterated medicines. Falsified medicines also have social and economic consequences. Patients’ confidence in their doctors, pharmacists as well as modern medicines is reduced. Patients who consume falsified medicines also suffer economic losses, as they spend their hard-earned income on ineffective medication [5]. The economic losses to individual income may be significant in developing nations, where medicines can constitute a substantial percentage of individual income (Laura Christiana, et al. 2012). Illness and death affect individual/family income and national economies, as they result in loss of productive man hours. Newton, et al. [33] further submitted that falsified medicines often lead to illness, additional costs for healthcare workers are incurred and the need to guard against falsified medicines further increases the cost for regulatory agencies and enforcement authorities. These regulatory costs may include personnel costs, healthcare workers, regulatory and enforcement agents, medical equipment costs, drug testing laboratories, and administrative costs (Laura Christiana, et al. 2012). Genuine manufacturers of pharmaceuticals are also adversely affected because they compete with illicit manufacturers of fake medicines, who do not pay import duties, and company sales tax for the fake medicines they sell thus negatively affecting the national economy [19]. Counterfeit and falsified medicaments discourage foreign direct investment (FDI) to the countries involved and reduce profits for developing nations by reducing incentives for further research and diverting resources for genuine treatment [22].
The majority of the respondents are of the view that government should declare a state of emergency on fake and adulterated medicines and its relationship with gender had no effect on respondent’s views. A declaration of a state of emergency on fake and adulterated medicines in the pharmaceutical sector of the Nigerian economy and hence on the drug distribution system is a task that should be urgently taken up because of the resultant loss of lives, reduction in life expectancy, patients maimed and deformed, a lot of resources lost by individuals, healthcare providers, manufacturers, the nation, and Nigeria’s image battered on the international scene, hence discouraging foreign direct investments (FDI).
This study has demonstrated the experiences of residents of Anambra, south-eastern Nigeria following the use of fake and adulterated medicines, their perceptions on the factors that enable their distribution and the social and economic impact of such medications as well as their suggestions on ways to curb this menace. The results of this study serve as a wake-up call to all regulating agencies in Nigeria: NAFDAC, Pharmacists Council of Nigeria (PCN), and Federal Ministry of Health (FMOH). The Government of Nigeria should make curbing fake and adulterated medicines a priority new and relevant laws that will control the sale of medicines and punishment for dealers of illicit medicines should be made, as a matter of urgency. Laws guiding the distribution of medicines in Nigeria should also be reviewed so that all the loopholes would be covered to enable the regulators to have all the necessary tools they require in order to regulate effectively. Regulators of fake and adulterated medicines should be empowered with both human and material resources to enable them to perform their responsibilities optimally.
- Akunyili DN. The War Against Fake Medicines: My Story. Safari Books Ltd. Ibadan. Cambridge House; 2010:19-27.
- Akunyili DN. Officials boost fight against counterfeit drugs. Available from: www.scienceafrica.co.za/2007/april/fakedrugs.htm; 2007.
- World Health Organization. Combating counterfeit drugs. Available from: https://www.aifa.gov.it/sites/default/files/111.118009.1140600148254b312.pdf; 2006.
- Newton PN, Green MD, Fernández FM, Day NP, White NJ. Counterfeit anti-infective drugs. Lancet Infect Dis. 2006 Sep;6(9):602-13. Available from: https://pubmed.ncbi.nlm.nih.gov/16931411/
- Nsimba SE. Problems associated with substandard and counterfeit drugs in developing countries: a review article on global implications of counterfeit drugs in the era of antiretroviral (ARVs) drugs in a free market economy. East Afr J Public Health. 2008 Dec;5(3):205-10. Available from: https://pubmed.ncbi.nlm.nih.gov/19374325/
- Hanif M, Mobarak MR, Ronan A, Rahman D, Donovan JJ Jr, Bennish ML. Fatal renal failure caused by diethylene glycol in paracetamol elixir: the Bangladesh epidemic. BMJ. 1995 Jul 8;311(6997):88-91. Available from: https://pubmed.ncbi.nlm.nih.gov/7613408/
- Dégardin K, Roggo Y, Margot P. Understanding and fighting the medicine counterfeit market. J Pharm Biomed Anal. 2014 Jan;87:167-75. Available from: https://pubmed.ncbi.nlm.nih.gov/23384475/
- Bate R, Ayodele T, Tren R, Hess K, Sotola O. Drug Use in Nigeria. 2009.
- All West Africa. West Africa Rallies against Counterfeits. 2010.
- International Council of Nurses. Counterfeits Kill; Nurses target counterfeit medicines. Available from: https://www.ordemenfermeiros.pt/arquivo/relacoesinternacionais/Documents/Organizacoes_Internacionais/ICN/Kit_DIE_2005_ing.pdf; 2005.
- Ten Ham M. Impact on patients. In: LePark M, editor. Protecting Medicines and Pharmaceuticals: A Manual of Anti-counterfeiting Solutions. Reconnaissance International: Greenwood Village, CO; 2002:21-24. Chapter 4.
- Deisingh AK. Pharmaceutical counterfeiting. Analyst. 2005;130:271-279. Available from: https://pubs.rsc.org/en/content/articlelanding/2005/an/b407759h
- Polgreen L. 84 Children Are Killed by Medicine in Nigeria. The New York Times. 2009. Available from: https://www.nytimes.com/2009/02/07/world/africa/07nigeria.html
- Eboh C. Nigeria Infant drug toll hits 34, antidote flown in. Reuters. 2008.
- Harris J, Stevens P, Morris J. Keeping it real: Combating the spread of fake drugs in poor countries. International Policy Network. Available from: https://www.africanliberty.org/wp-content/uploads/Keepingitreal.pdf; 2009.
- Mbachu D. Nigeria tainted Syrup Kills 84 Children; drug still selling. Bloomberg.com. 2009 Feb 6. Medine. 2(2).
- Milissa McGinnis MA. Matrix of Medicine Quality Reports Affecting USAID assisted Countries by the Promoting the Quality of Medicines program. 2010.
- World Health Organization. The quality of Antimalarials: A Study in Seven African Countries. Geneva, Switzerland: World Health Organization; 2003. Available from: https://iris.who.int/handle/10665/68053
- Fenoff RS, Wilson JM. African's Counterfeit Pharmaceutical Epidemic: The Road Ahead. 2009. Available from: https://www.ojp.gov/ncjrs/virtual-library/abstracts/africas-counterfeit-pharmaceutical-epidemic-road-ahead
- Agege CO. Products and the consumers: An analysis of food and drug legislation in Nigeria. Hein online Food and drug law Journal. 1988;43:201.
- Okeke TA, Uzochukwu BS, Okafor HU. An in-depth study of patent medicine sellers' perspectives on malaria in a rural Nigerian community. Malar J. 2006;5:97. Available from: https://pubmed.ncbi.nlm.nih.gov/17078875/
- Lybecker KM. Rx Roulette: Combating Counterfeit Pharmaceuticals in Developing Nations. Managerial and Decision Economics. 2007;28:509-520. Available from: https://ideas.repec.org/a/wly/mgtdec/v28y2007i4-5p509-520.html
- Ofomata CM. Effects of Fake and Adulterated Medicines on Nigerians. A PhD Thesis submitted to the International School of Management (ISM), Paris, France. 2018.
- Olike C. The fight against fake drugs by NAFDAC in Nigeria. Paper presented at the 44th International Course in Health Development (ICHD), September 24, 2007―September 12, 2008. KIT (Royal Tropical Institute) Development Policy & Practice/ Vrije Universiteit Amsterdam. Available from: https://www.bibalex.org/Search4Dev/files/353722/193922.pdf
- Prazuck T, Falconi I, Morineau G, Bricard-Pacaud V, Lecomte A, Ballereau F PhD. Quality control of antibiotics before the implementation of an STD program in Northern Myanmar. Sex Transm Dis. 2002;29:624-627. Available from: https://journals.lww.com/stdjournal/abstract/2002/11000/quality_control_of_antibiotics_before_the.2.aspx
- Erhun WO, Erhun MO, Babalola OO. Drug Regulation and Control in Nigeria: The challenge of counterfeit drugs. J Health Popul Dev Ctries. 2001;4(2):23-34. Available from: https://nairametrics.com/wp-content/uploads/2013/02/Drug_regulation-and-control-in-Nig.pdf
- Akunyili DN. Fake and counterfeit drugs in the health sector. Ann Ibadan Postgrad Med. 2004;2:19-23.
- Mackey TK, Liang BA. Improving global health governance to combat counterfeit medicines: a proposal for a UNODC-WHO-Interpol trilateral mechanism. BMC Med. 2013;11:233. Available from: https://pubmed.ncbi.nlm.nih.gov/24228892/
- Kron MA. Substandard primaquine phosphate for US Peace Corps personnel. Lancet. 1996;348:1453-1454. Available from: https://pubmed.ncbi.nlm.nih.gov/8937304/
- Kao SL, Chan CL, Tan B, Lim CC, Dalan R, Gardner D, et al. . An unusual outbreak of hypoglycemia. N Engl J Med. 2009 Feb 12;360(7):734-6. Available from: https://pubmed.ncbi.nlm.nih.gov/19213693/
- Blackstone EA, Fuhr JP Jr, Pociask S. Intellectual property: facts and consumer opinions on counterfeit and pirated goods. American Consumer Institute. 2013 Jul 25. Available from: https://www.theamericanconsumer.org/wp-content/uploads/2013/07/Final-IP-Study-w-Cover.pdf
- Liang BA, Mackey TK. Sexual medicine: Online risks to health--the problem of counterfeit drugs. Nat Rev Urol. 2012 Sep;9(9):480-2. Available from: https://pubmed.ncbi.nlm.nih.gov/22824776/
- Newton PN, Green MD, Fernández FM. Impact of Poor-Quality Medicines in the 'Developing' World. Trends Pharmacol Sci. 2010;31:99-101. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20117849.
- Akunyili D. Counterfeit and Substandard Drugs, Nigeria’s Experience: Implications, Challenges, Actions And Recommendations. Speech delivered at a meeting for key interest groups on health organized by the World Bank in Washington DC; 2005.
- Bate R, Porter K. American Enterprise Institute Health Policy Outlook No. 3: The Problems and Potential of China's Pharmaceutical Industry. Washington, D.C.: American Enterprise Institute; 2009. Available from: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2342849
- World Health Organization. Counterfeit Medicines. Fact Sheet. 2006. Available from: http://www.who.int/mediacentre/factsheets/fs275/en/.
- Newton PN. Murder by Fake Drugs in SE Asia- Prevalence and Prevention. In: Proceedings of the Global Forum on Pharmaceuticals Anti-Counterfeiting; 2002. Geneva, Switzerland: Egham, UK: Reconnaissance International.