More Information
Submitted: July 15, 2024 | Approved: July 24, 2024 | Published: July 26, 2024
How to cite this article: Maparu K. Modulation of Microbiota and its Impact on Depression. Arch Pharm Pharma Sci. 2024; 8(1): 089-090. Available from:
https://dx.doi.org/10.29328/journal.apps.1001061
DOI: 10.29328/journal.apps.1001061
Copyright License: © 2024 Maparu K. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction inany medium, provided the original work is properly cited.
Keywords: Probiotics; Depression; Gut-brain axis
Modulation of Microbiota and its Impact on Depression
Kousik Maparu*
ISF College of Pharmacy, Moga, Punjab-142001, India
*Address for Correspondence: Kousik Maparu, ISF College of Pharmacy, Moga, Punjab-142001, India, Email: [email protected]; [email protected]
Gut microbial flora is the largest micro-ecosystem in the human body, it is symbiotically associated with the host; and maintains normal physiological processes in a dynamic equilibrium state. A plethora of evidence supports that gut microbial flora influences the neurotransmitters of the central nervous system. This gut flora influences cognitive function, anxiety, depression; and mood disorders as they are capable of synthesizing neurotransmitters in the nervous system. Therefore intake of probiotics influences gut microbiome; and depression. The versatility and number of gut microbial flora varies individually, so the content of common gut microbes may affect the neurotransmitters, manipulating the gut microbiota with probiotics offers a novel approach to treat brain disorders such as depression via GUT-BRAIN AXIS. The present review outlines the aspect of such alterations and how modulation of gut microbiota influences depression.
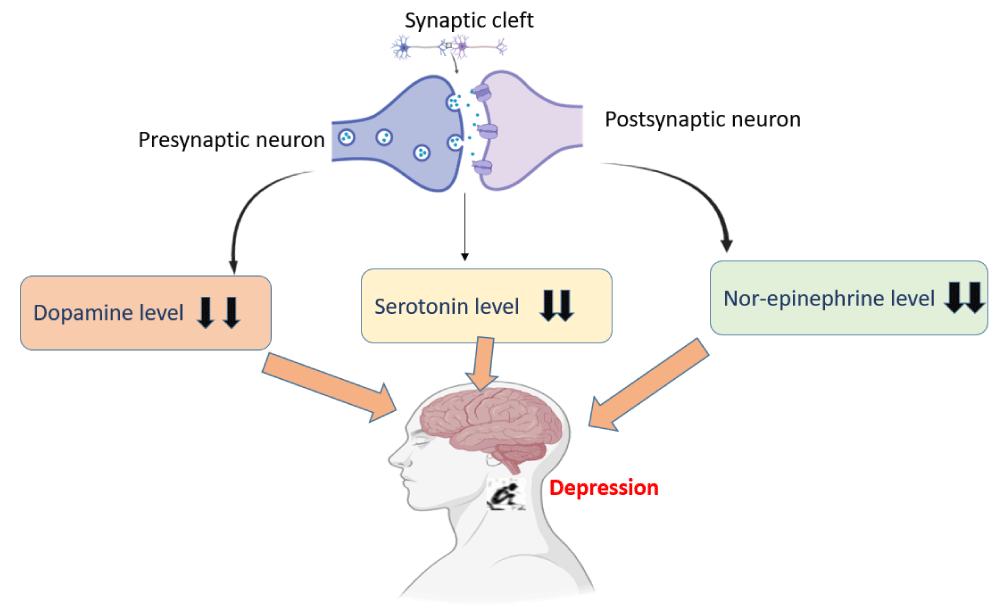
Gut microbial flora is the largest micro-ecosystem in the human body, it is symbiotically associated with the host and maintains normal physiological processes in a dynamic equilibrium state [1]. The human microbiome known as a ‘forgotten organ’ has been elevated to importance in a wide array of host processes such as growth, development, immunity, and many more and the gut microbiome is a dynamic, referred to as, a ‘necessary and ever-changing organ’ [2]. A plethora of evidence supports that gut microbial flora influences the neurotransmitters of the central nervous system. This gut flora influences cognitive function, anxiety, depression, and mood disorders as they are capable of synthesizing neurotransmitters in the nervous system [3]. Depression is a common and serious mental illness that involves various neurotransmitters in the CNS as shown in Figure 1.
Figure 1: Involvement of neurotransmitters in depression.
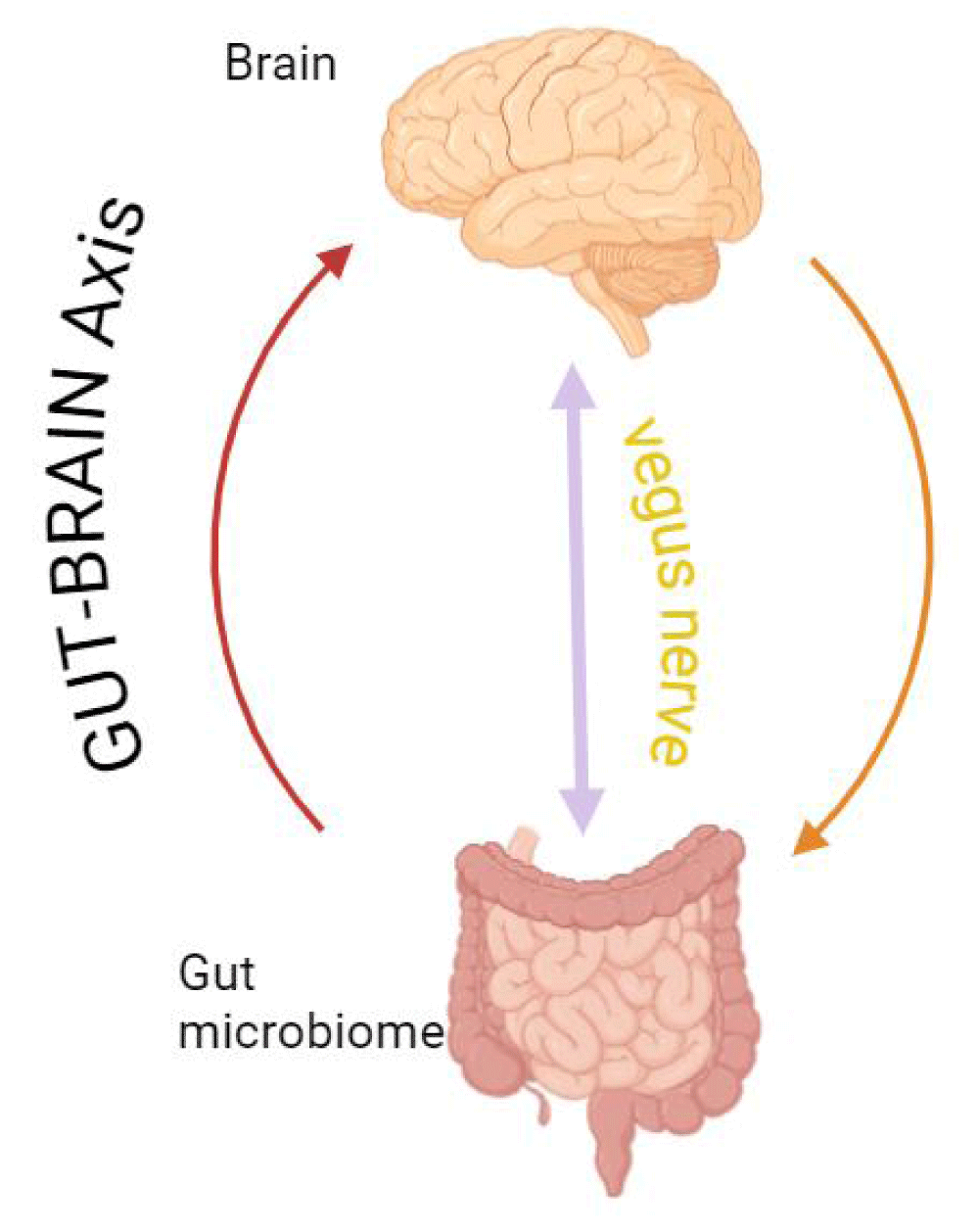
Probiotics may induce changes in the intestinal microbiota and stabilize the microbial community [4]. Therefore intake of probiotics influences gut microbiome and depression. Versatility and number of gut microbial flora varies individually, so the content of common gut microbes may affect the neurotransmitters, manipulating the gut microbiota with probiotics offers a novel approach to treat brain disorders such as depression via GUT-BRAIN AXIS [5] (Figure 2).
Figure 2: Connection of gut-brain axis.
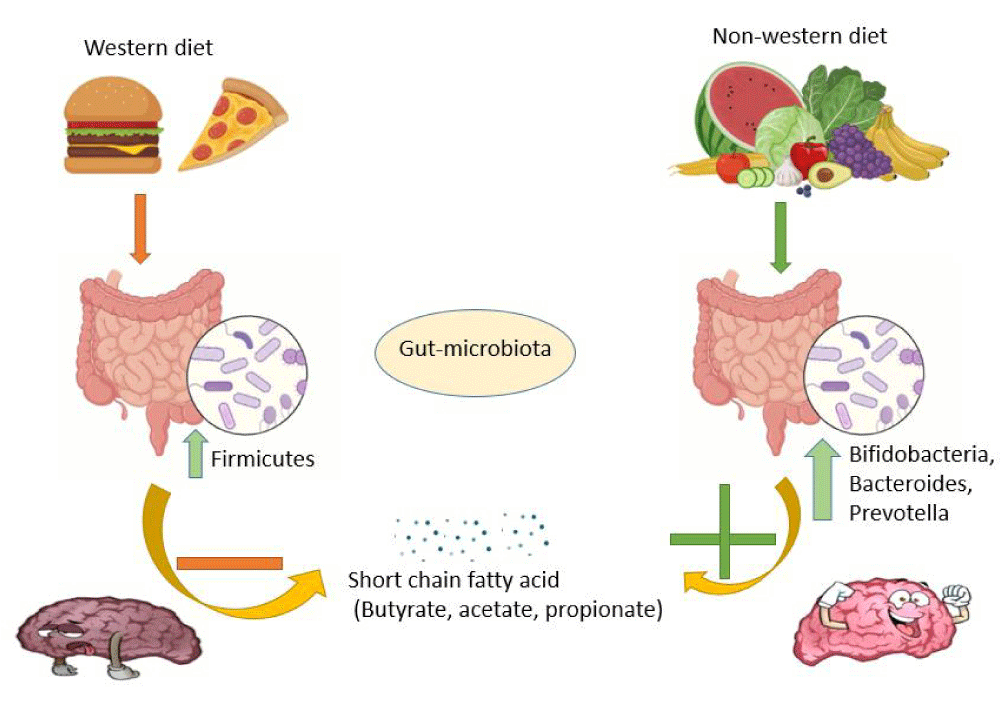
Gut microbes may communicate with the gut-brain axis via the production of neuroactive and neuroendocrine molecules such as serotonin, GABA, Histamine, adrenaline noradrenaline via the vagus nerve (composed of 80%afferent and 20% efferent nerve) [3,6]. The gut response comes into the brain via the vagus nerve and reduces depression. Ingestion of probiotics bacteria changes the microbial content of GUT and triggers a very protective pathway related to depression. Various lifestyles and foods are involved in brain health via gut microbiota by regulating various good and bad microorganisms, and involving various short-chain fatty acids [7] (described in Figure 3). Depression can be treated by the use of psychotherapy and probiotics and it could be the first line of treatment before switching to pharmaceutical drugs like selective serotonin reuptake inhibitors. Probiotics can be the natural solution to mental health crises and replace pharmaceuticals as the standard of care [8].
Figure 3: Food and lifestyle involved in brain health via gut microbiota.
In many medical diseases, such as depression, psychiatric medication reactions, pregnancy, irritable bowel syndrome (IBS), and autism, the gut-brain axis plays a critical role [9]. It has been discovered that SSRIs, such as fluoxetine, are beneficial in helping IBS patients with their psychological and gastrointestinal problems [10]. The development of the gut-brain axis in fetuses can be impacted by pregnancy and mental medication use. Probiotics have the potential to improve brain health by preventing the transfer of hazardous biomolecules and show promise in the treatment of diseases like necrotizing enterocolitis in babies [11]. This axis affects illnesses like obesity, multiple sclerosis, and Parkinson’s disease and has an impact on health from childhood to adulthood [12]. The gut microbiota-dysbiosis model of depression suggests that the development of depressive-like behaviors is probably influenced by the gut microbiota. This includes affecting how the gut-brain axis functions and how proteins are expressed, especially with regard to energy metabolism. These results provide new perspectives for investigating the gut-brain axis at the protein level in the future, which will help us better understand how gut microbiota influences behaviors associated with depression.
A growing body of data indicates that the gut-brain axis is implicated in depression, and probiotics appear to be a promising therapeutic intervention. Probiotics may assist in modifying the composition of the gut microbiota, which may have an impact on mood and symptoms of depression via interacting with the central nervous system. Although further research is required to determine the best probiotic strains and dosages for treating depression and to completely understand the underlying mechanisms, the promising potential of probiotics in managing depression through gut-brain axis modulation is already evident.
- Chen Y, Zhou J, Wang L. Role and Mechanism of Gut Microbiota in Human Disease. Front Cell Infect Microbiol. 2021;11:625913. Available from: https://doi.org/10.3389/fcimb.2021.625913
- Ling Z, Xiao H, Chen W. Gut Microbiome: The Cornerstone of Life and Health. Adv Gut Microbiome Res. 2022;2022(1):9894812. Available from: https://doi.org/10.1155/2022/9894812
- Appleton J. The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health. Integr Med (Encinitas). 2018;17(4):28-32. Available from: https://pubmed.ncbi.nlm.nih.gov/31043907/
- Hemarajata P, Versalovic J. Effects of probiotics on gut microbiota: mechanisms of intestinal immunomodulation and neuromodulation. Ther Adv Gastroenterol. 2013;6(1):39-51. Available from: https://doi.org/10.1177/1756283x12459294
- Chaudhry TS, Senapati SG, Gadam S, Mannam HPSS, Voruganti HV, Abbasi Z, et al. The Impact of Microbiota on the Gut-Brain Axis: Examining the Complex Interplay and Implications. J Clin Med. 2023;12(16):5231. Available from: https://doi.org/10.3390/jcm12165231
- Dicks LMT. Gut Bacteria and Neurotransmitters. Microorganisms. 2022;10(9):1838. Available from: https://doi.org/10.3390/microorganisms10091838
- Conlon MA, Bird AR. The impact of diet and lifestyle on gut microbiota and human health. Nutrients. 2014;7(1):17-44. Available from: https://doi.org/10.3390/nu7010017
- Jach ME, Serefko A, Szopa A, Sajnaga E, Golczyk H, Santos LS, et al. The Role of Probiotics and Their Metabolites in the Treatment of Depression. Molecules. 2023;28(7):3213. Available from: https://doi.org/10.3390/molecules28073213
- Dinan TG, Cryan JF. The Microbiome-Gut-Brain Axis in Health and Disease. Gastroenterol Clin North Am. 2017;46(1):77-89. Available from: https://doi.org/10.1016/j.gtc.2016.09.007
- Creed F. How do SSRIs help patients with irritable bowel syndrome? Gut. 2006;55(8):1065-7. Available from: https://doi.org/10.1136/gut.2005.086348
- Clarke G, Grenham S, Scully P, Fitzgerald P, Moloney RD, Shanahan F, et al. The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Mol Psychiatry. 2013;18(6):666-73. Available from: https://doi.org/10.1038/mp.2012.77
- Gianfrancesco MA, Barcellos LF. Obesity and Multiple Sclerosis Susceptibility: A Review. J Neurol Neuromedicine. 2016;1(7):1-5. Available from: https://doi.org/10.29245/2572.942x/2016/7.1064